Building better health: exploring opportunities for healthcare estate under integrated care systems
31 August 2022
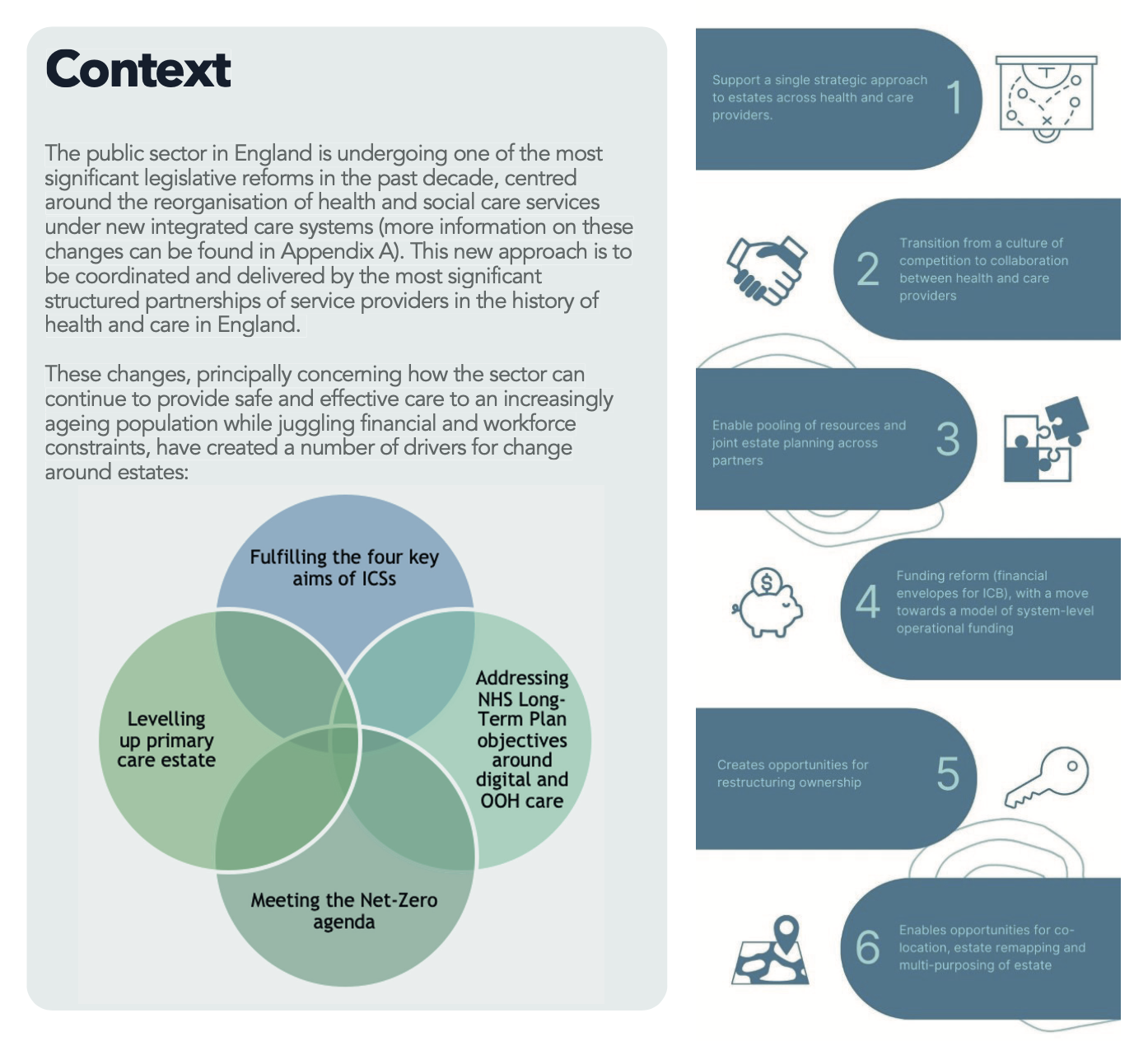
What are the estate development and management opportunities presented by integrated care systems?
A roundtable discussion facilitated by the Good Governance Institute and Primary Health Properties.
Introduction
The Good Governance Institute and Primary Health Properties have partnered to conduct research into the opportunities for healthcare estate, particularly primary community and outpatient, development, and reconfiguration under integrated care systems(ICSs). On 13 July 2022, GGI and PHP hosted a roundtable event with a selected group of senior decision-makers in health and social care to discuss the potential that estates have for driving reform, innovation and improvement (a list of attendees can be found at Appendix B).
The roundtable discussion focused on ways in which developing or repurposing NHS estate can enable co-location and, in time, integration of health and care services. The discussion included an exploration of the benefits, success factors and drivers of estates development. Before the event GGI and PHP had conducted interviews with 15+ senior estates leads from trusts and ICSs exploring opportunities and challenges around the above, with co-location of services consistently identified as one of the most significant opportunities.
The session was chaired by Simon Crick, a senior consultant at the Good Governance Institute and former NHS finance director with years of experience with estate development across various NHS organisations. Tony Coke, director of primary care development for Primary Health Properties provided a contextual overview of his work and the opportunities for estate as an enabler of change. A case study of co-location in practice – the Thurrock Locality Integrated Medical Centres in Mid and South Essex Integrated Care System - was presented by the guest speaker, Kerry Harding, to frame the discussion.
Key takeaways
- There are huge opportunities for estate management and development in ICSs.
- Strategic estate management and development will play a key role in determining the extent to which ICSs are able to meet their aims, as well as acting as a key enabler to care model innovation.
- Co-location provides a wealth of opportunity to drive integration, achieve cost efficiencies and improve patient care and the Integrated Medical Centre approach in Mid and South Essex provides a strong example upon which services can be modelled.
- Closer working with partners, especially between providers and local authorities, will be vital to ensuring that community and primary estate is optimised, rationalised and used most effectively.
- The importance of softer elements such as culture and behaviours should not be underestimated and are often as important, if not more so, than optimal estate in driving integration of services. Aligning these should be prioritised at an early stage.
- There is not yet strong academic evidence upon which to base decisions around estates utilisation and optimisation so current practitioners are having to take a common-sense approach to the design and development of new facilities. Through this process, it is important that good practice is shared and built upon.
Chair’s opening remarks – Simon Crick
Simon kicked off the session by introducing the purpose of the roundtable – to explore the opportunities ICSs present for estates development and management. He spoke about his own experience with healthcare estate as a former NHS finance director, including commissioning a new PFI hospital.
Simon also reflected on the time he spent working for the Police Crime Commissioner and the volume of redundant police estate that just wasn't being used: “I had some amazing visits where I'd turn up at a six-storey tower block, and the first floor there'd be some policemen doing various bits and some back-office staff and the rest of the building would be completely empty and not be used for anything. Unfortunately, there wasn't the knowledge and capacity in the police force to deal with that, so we entered into a strategic property partnership with the county council and a private partner to help rationalise that to make better use and reinvest it back into public services.”
He wrapped up his opening remarks by introducing the two speakers - Tony Coke from Primary Health Properties and Kerry Harding from Mid and South Essex ICS.
Estates as a healthcare enabler - Tony Coke
Tony started by introducing PHP as one of the largest owners of primary care estate outside of the NHS, with 511 sets of properties up and down the country.
He spoke about his role at PHP, as head of development on PHP’s third-party developer offer, reflecting that his work had shifted recently to system-type projects with the trusts holding the lease and offering integration of services through the various occupiers.
This increase in system-focused projects, Tony explained, is what brought PHP into partnership with GGI thinking about the changes ICSs would bring – “What genuinely is the direction of travel? Where do these organisations see their estate going?”
Tony emphasised how PHP wanted to ensure that its estate was meeting the needs of its occupiers in as full a way as possible, that it was attuned to the needs and strategic priorities of commissioners, and, finally, that it was alive to the opportunities in estate development under ICSs: “What we're keen to understand is, what that looks like, how you would see commissioning that, and how you would like us to respond to it.”
‘Doing the most with the least’: Integrated Medical Centres - Kerry Harding
Kerry’s presentation focused on her experience of leading the development of several ‘Integrated Medical Cen- tres’ (IMCs), multipurpose facilities designed to provide better access to services and deliver better outcomes for those in Mid and South Essex.
She began by discussing the journey that Mid and South Essex ICS had been on in developing four Integrated Medical Centres across Thurrock which are key components of achieving the ICS’s aims of delivering improved care within local communities and, in particular, delivering more out of hospital services closer to home.
Kerry highlighted how the IMCs had the potential to improve efficiency, drive greater estate utilisation and, perhaps more surprisingly, improve recruitment and retention: “We're hoping that these will support recruitment and retention by providing fit for purpose estate, within our community, by bringing services together, we give people a much better environment to work, we make our staff much happier. And also, they have the opportunity for training, and coming into the system and looking at where they might want to go in the future, and maybe a new career.”
She also underscored the importance of considering the sustainability and accessibility implications when develop- ing or re-developing estate, arguing that “it [new and existing estate] must be cost-effective, not just in terms of the bills, but the running cost and longer term. We also have to make sure that we're achieving our net-zero carbon targets,” and “of course, all of these properties have to be accessible, and that's not just accessible in terms of the design, how we set services out and how the pathways run throughout the buildings, but actually where they're located to make sure we've got access from public transport and other sustainable transport meth- ods, including walking and cycling – that's just one of many areas where the close working partnership with local authorities is so important and such a lever for positive change.”
Summing up this work, Kerry encapsulated the core estates challenge for all ICSs: “Essentially what we're trying to do with Integrated Medical Centres is doing the most with the least within our community and freeing up monies wherever we can to provide more services rather than spending money on dilapidated estate.”
In Mid and South Essex, these developments were set against the broader work that the ICS had been conducting to improve its community estate, which had included taking stock of existing estate across the system and agree- ing what, strategically, could be brought together, what could be reused and repurposed, and what needed refurbishment or upgrading. This process, Kerry said, had facilitated more joined up and purposeful estate ratio- nalisation and disposal. As Kerry pointed out: “We're not looking simply at just disposing to give us capital; we're looking at where those disposals might be able to help with other services within the community... we assess all of our options, all the opportunities.”
Kerry’s four lessons from the Mid and South Essex experience
- “Councils have been brilliant and willing partners with us, but they've not been able to meet the lease terms that we need due to affordability. Basically, when we're looking at community estate, we're still working on value for money in terms of the district valuer’s opinion of value, and the councils need to look at full cost recovery, which doesn't always add up. So, although we're still trying to work through, that's been something that we probably could have addressed slightly earlier on in the process.”
- “You must have your service model first. Obviously, that's been difficult. Things have changed very, very quickly. We've been looking at IMCs for the last five years, but I think it's absolutely key that you have a service model that is flexible, and that that's what you stick with. That the design agreed is what you start with and what you end with. If the service configuration changes in between, just make sure that the building is flexible in terms of design and operation. So, if the service actually does change in the community, it doesn't have any effect on the design of the property.”
- “And, of course, being realistic. You have to be really careful with messaging. Integrated Medical Centres are absolutely brilliant, they're going to be a huge benefit to the community. But these properties are not cheap. They do follow full Green Book process, which is timely and costly. As soon as you start to tell the public that we're building these centres, they expect to see them within the next year or two, and obviously, this is not always possible. And if we're moving services, then there's a lot of work to be done with the community in terms of engagement and consultation.”
- “Lastly, then understanding the constraints, some of the properties or the services moving in may have leases that we have to wait for an end from, so you may have to phase a building. In summary, we need to develop a model that has the flexibility to adapt to the demographics and the changing health and care landscape. That's not only for while we're developing and delivering, but also the next 20-40-60 years to come.”
Kerry’s four key challenges from the Mid and South Essex experience
- “One of the main challenges has been CDEL. If you're going to build something bigger and better, ultimately the capital value is more. We're struggling at the moment to understand how we can deal with CDEL, how are we going to deliver four Integrated Medical Centres, how we're going to bring those onto the books because we can't dispose of existing properties until we've built new ones, and then how we're going to deal with that, not only in terms of capital to build - in some instances, we have got third parties building for us - but it's now the lease issue that we have because of IFRS 16, and that obviously gives us a CDEL impact too.”
- “Facilities management is another. If we are going to own a building either as an ICB or one of our partner organisations, we're not currently set up for building facilities management in the community. So,
it's trying to understand how we could commission that. I'm currently working with EPUT and some other trusts to see whether we could develop something centrally and have our own offering within the community as an ICS for building and facilities management, but that's going to take time. At the moment, we're looking at third party contracts to be able to deliver the building so that we have the same consistency of delivery and building maintenance throughout the building, regardless of whether areas belong to the Council, or to the NHS or to outside providers.” - “Also building management systems. Within my area particularly, we're not great at building management systems within community estate. That's something we need to look at so we can start to get a handle on how our buildings are working, how we can make them more efficient, and how they're delivering for us, a simple dashboard across the whole community, which is going to be quite a big task in itself.”
- “Lastly, identifying the head leaseholder and management of sub-occupancies. At the moment a trust may take the whole lease but, of course, we don't have the CDEL cover. The Council are not willing, or have the ability currently, to hold the lease and manage all of the individual sub occupancies because they don't have the capacity to do so. As an ICB, if we did hold the head lease, again, we don't have the capacity or the mechanism set up internally to manage these buildings in terms of sub-occupancies. So, there's going to have to be a change in the way that we work as well. They're all things that we're trying to work through currently.”
Highlights from the discussion
Following Kerry’s presentation, the roundtable was then opened to group discussion, which focused on:
- potential benefits of co-locating teams
- key success factors for co-location
- drivers for co-locating services.
1. Potential benefits of co-locating teams
The discussion identified that co-locating teams can improve both the patient and staff experience as well as lead to improved productivity and value for money (see table below).
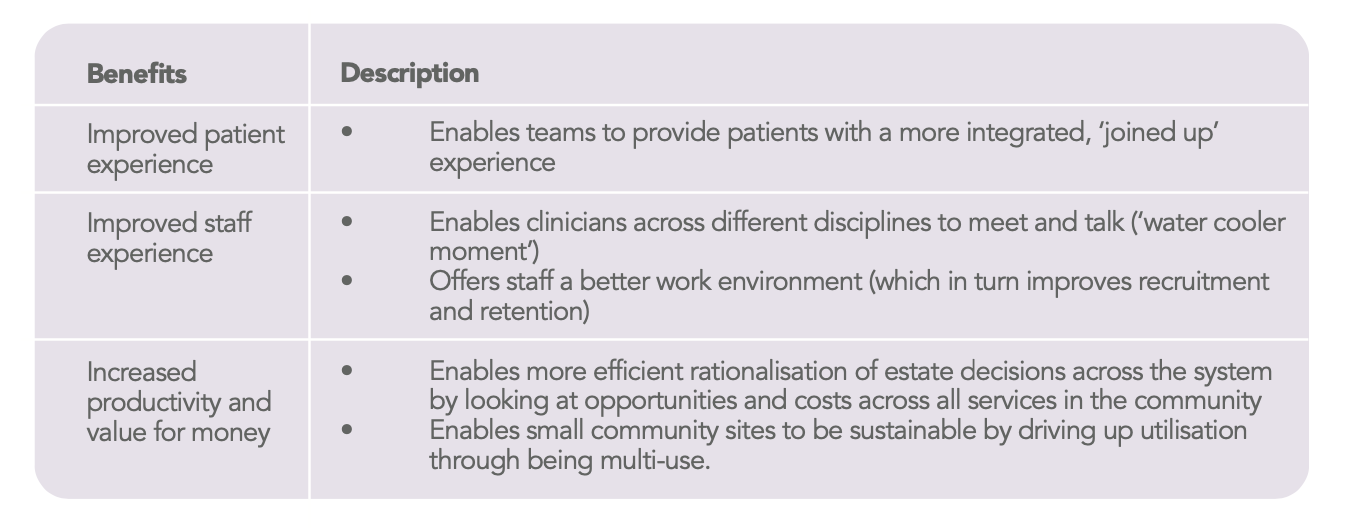
The Crick Institute in London is a research institute and an example of successful multi-disciplinary working. It is a unique partnership between six world leading biomedical research organisations that brings a variety of clinicians, physical scientists and applied scientists to work together with no divisions or departments.
2. Key success factors
The discussion identified several key success factors for co-location:
- building the business case
- involving stakeholders
- training staff
- communicating with patients
- providing estate management training
Building the business case
Business cases should be anchored in a clinical care model, include evidence-based assumptions, and focus on the long term – this latter point is a particular challenge for the NHS, which operates on annual budget cycles.
“We have an Integrated Infrastructure and Investment Group in our ICS. We are creating an integrated infrastruc- ture and investment plan that covers all areas - primary, community, mental health and acute and digital. Really important for a rural county to look at what capacity we need where to reduce inequalities and meet clinical needs."
Involving stakeholders
Involving stakeholders, such as primary care, in the design helps ensure that they are “fit for purpose and provide best value to clinicians and patients” (director, Heart of England, large CCG).
When co-locating teams across health and social care, local councils should be fully involved as partners.
Engagement and consultation with the local community is essential so that expectations can be managed and the public can be reassured that services will not be adversely impacted.
Training staff
It’s behaviours, not the co-location in itself, that creates value: “You can build the best building in the world, but it's the behaviours of the people in the building that make a difference as to whether it has an impact.”
Training should start with agreeing expectations, identifying shared values and establishing aligned ways of working at the outset between partners.
Some training needs to focus on aligning differences in working arrangements: “Cultural differences between various practitioners have resulted in the underusage of certain rooms and services.” (North, GP practice).
Some suggested that behaviour programmes should be an essential requirement, e.g. “You’re only allowed to move into the new building if you’re going to do things differently.” (Innovator, South medium-sized ICS).
Some changes in behaviours may need to be supported by the provision of technology or equipment.
Communicating with patients
Some communication and education may also be required for patients: “It's not actually about bricks and mortar...it's about people, and that's both staff, patients, etc.” (NED, South, large community Trust).
Providing training non estate management skills
It would be very relevant for some training to include effective estate and facilities management and procurement skills. This could include concepts such as how to:
- future-proof estate design that is flexible enough to cope with changes to demographics and service models)
- provide incentives for people to move into buildings
- ensure that estate design is accessible and sustainable long term.
3. Drivers of successful co-location
A key driver for co-location in primary care is the consolidation of GPs into single sites. A key driver for re-purpos- ing and re-orientating existing estate portfolios is service reconfiguration, enabled by the application of digital technologies: “There's a huge amount that can be done by not having buildings and focusing on things that we can do without buildings...virtual wards, all that sort of thing.” (NED, South, large community Trust).
Concluding thoughts
The discussion at the roundtable highlights the increasingly important role that creative and considered estate management can play in helping to achieve the ICS aims. The discussion identified benefits for patients and staff, as well as opportunities to increase productivity and value for money.
Key success factors were explored from building the business case, to involving stakeholders to training and communication with staff and patients. In particular, a potential accelerator for success is providing training on estate management skills. Key drivers for co-location and repurposing of real estate such as GP consolidation and service reconfiguration (often driven by the application of digital technologies) were also highlighted.
Health and social care estate management is likely to grow in impact and importance. It is increasingly recognised as a key enabler for improving health outcomes, reducing inequalities, increasing productivity, and contributing to the socio-economic health of communities (the ICS aims).
About GGI & PHP
The Good Governance Institute (GGI)
The Good Governance Institute (GGI) exists to help create a fairer, better world. Our part in this is to support those who run the organisations that will affect how humanity uses resources, cares for the sick, educates future generations, develops our professionals, creates wealth, nurtures sporting excellence, inspires through the arts, communicates the news, ensures all have decent homes, transports people and goods, administers justice and the law, designs and introduces new technologies, produces and sells the food we eat - in short, all aspects of being human.
We work to make sure that organisations are run by the most talented, skilled and ethical leaders possible and work to build fair systems that consider all, use evidence, are guided by ethics and thereby take the best deci- sions. Good governance of all organisations, from the smallest charity to the greatest public institution, benefits society as a whole. It enables organisations to play their part in building a sustainable, better future for all.
Find out more: https://www.good-governance.org.uk/
Primary Health Properties (PHP)
Primary Health Properties (PHP) is a UK real estate investment trust (REIT) and leading investor in modern primary healthcare premises.
PHP has invested over £2.9bn in the primary care estate since its inception 26 years ago, including by refurbishing or reconfiguring existing buildings or via the delivery of new purpose-built buildings to meet the evolving needs of primary care.
PHP’s portfolio comprises 512 primary healthcare facilities valued at £2.9 billion. Most are GP surgeries, with other properties let to NHS organisations, pharmacies and dentists. PHP invests in flexible, modern properties. The company’s overall objective is to create progressive returns to shareholders through a combination of earnings growth and capital appreciation.
To achieve this, PHP has invested in healthcare real estate let on long-term leases, backed by a secure underlying covenant where the majority of rental income is funded directly or indirectly by a government body.
More: https://www.phpgroup.co.uk/
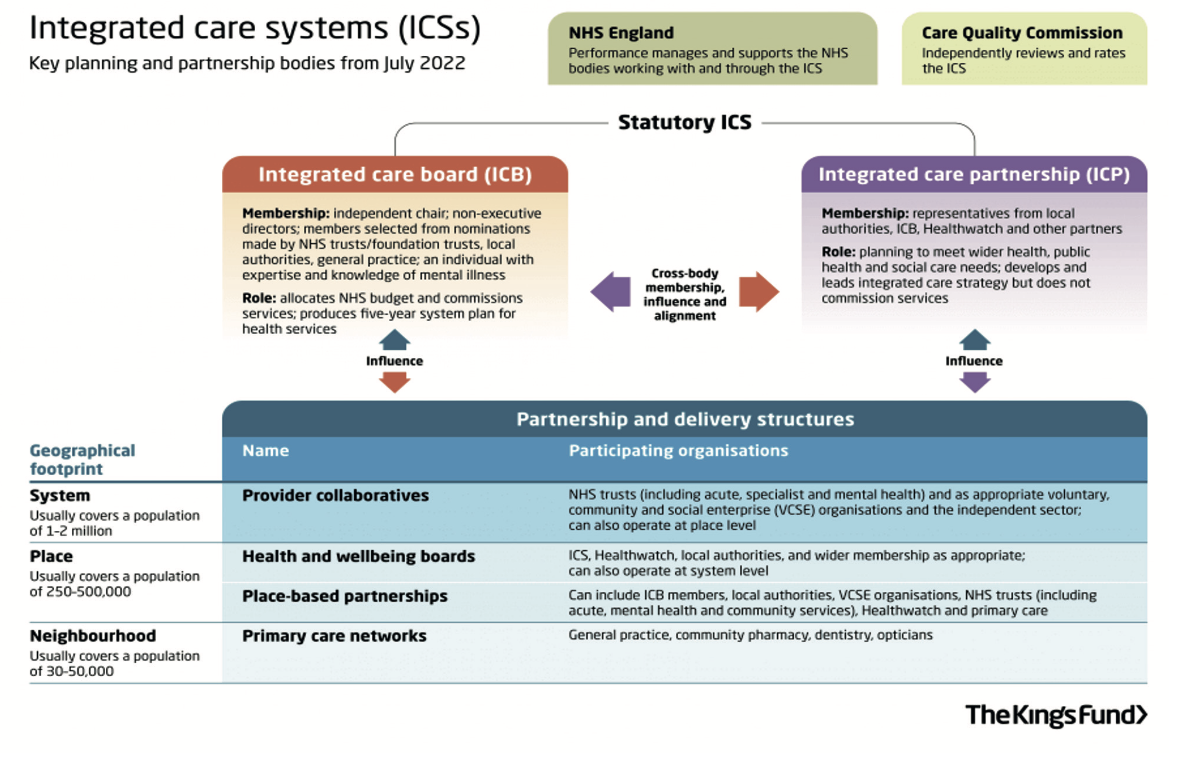
Appendix A: Background on integrated care systems
On 1 July 2022, all of the remaining clinical commissioning groups (CCGs), established under the Health and Social Care Act 2012, transitioned into new integrated care systems (ICSs), under the Health and Care Act 20221.
Signalling a departure from the competition model of the Lansley reforms, England is now formally divided into 42 ICSs – geographically based partnerships that bring together both providers and commissioners of NHS services along with local authorities, VCSE organisations and other local partners to collaboratively plan, co-ordinate and commission health and care services.
Each ICS covers a population of between 500,000 to 3 million people, and, through their NHS statutory bodies – the integrated care board – absorb the commissioning and funding responsibilities of the former CCGs alongside broader responsibilities focused on addressing health inequalities, enhancing productivity and value for money, and improving access and patient outcomes.
This new approach is to be coordinated and delivered by the most significant structured partnerships of service providers in the history of health and care in England.
Fig 1: The integrated care system
Appendix B: Attendance List
Chair
Simon Crick, Senior Consultant, Good Governance Institute
Speakers
Tony Coke, Director of Primary Care Development, Primary Health Properties Kerry Harding, Estates Director, Mid and South Essex Integrated Care System
Attendees
Jacqui Bunce, Programme Director for Estates, Lincolnshire CCG
Sheila Addison, GP Premises & Estates Support Manager, East and North Hertfordshire CCG
Grace Cowie, Programme Support Officer, ANHH Consulting Ltd
David Cryer, Executive Director of Strategy at Sussex CCGs, Sussex Health and Care Partnership ICS
Colin Greaves, Lay Member, NHS Gloucestershire CCG
Geoff Jolliffe, Chair, Morecambe Bay CCG
Oliver Judges, Non-Executive Director, Cambridgeshire Community Services NHS Trust
Kathryn McDermott, Deputy Director of Estates, Facilities & Capital Planning, Wirral University Teaching Hospital NHS Foundation Trust
Neil Mcelduff, Estates Programme Director, Birmingham and Solihull ICS
Peter Ramrayka, Lay Member, Lewisham CCG
Dag Saunders, Member of Shropshire, Telford & Wrekin Joint Health Scrutiny Committee, Telford and Wrekin Council
Daniel Taylor, Engagement Consultant, Good Governance Institute
Alison Tonge, Director for Integrated Service Development, Arden and Greater East Midlands Commissioning Support Unit
