Provider collaborative development: cultivating key system relations
03 January 2024
GGI consultant Daniel Taylor on why strategic engagement and attending to relationship management, information flows and connectivity will be crucial to the development of provider collaboratives.
Provider collaboratives sit at the heart of integrated care systems, bringing together healthcare providers to share resources, optimise care pathways, and improve population health outcomes while providing better value for money.
And one of the key success factors for provider collaboratives is engaging with stakeholders across systems and developing key relations and information flows with them.
The value and role of provider collaboratives
In her review of integrated care systems, the Rt Hon Patricia Hewitt, former health secretary and current chair of Norfolk and Waveney ICB, called collaboratives the delivery arm of systems and an ‘important engine of improvement and transformation’. She added:
“Collaboratives can bring together providers to improve access and reduce wait times, share best practice, staff and resources, and help overcome organisational barriers that can sometimes stop services from being designed and delivered around the needs of patients and communities. While provider collaboratives, like ICBs, vary considerably in maturity and strength, they have the potential to become the core NHS delivery arm for achieving key system objectives.”
Mature provider collaboratives will deliver a number of positive outcomes, including:
- Efficiency gains: collaboratives can optimise resource allocation, reduce duplication of services, and streamline administrative processes, leading to cost savings and improved efficiency.
- Strengthened partnerships: collaboratives foster stronger relationships and collaboration between providers, creating a more cohesive and coordinated healthcare system.
- Enhanced population health: collaboratives can focus on addressing the broader determinants of health, such as social determinants and preventive care, leading to improved population health outcomes.
Some guiding principles GGI has applied in our work supporting provider collaboratives, and have noticed in the DNA of more mature collaboratives, are:
- Patient benefits focus: changes in service design, processes and structures should only be made if they result in benefits to patients and residents.
- Focus governance arrangements on governance outcomes: governance arrangements should create improvements for ethical culture, adding value, better control and legitimacy.
- Subsidiarity: decision-making should be delegated to the most local level possible, with system-level decisions restricted to those that need to be made at scale.
- Form follows function: focus should remain on shared objectives and identifying the required interactions to achieve them; decisions on structures should come last.
- Simplicity: the temptation to label ordinary management or communication forums as ‘governance’ should be resisted. Only that which needs to be governed should be governed.
At the heart of all of these principles are establishing the right connections, relationships, flows of information, involvement of key stakeholders in decision-making and strategy development, managing system dynamics and building trust. All of these outcomes should be the focus of strategic engagement activity.
Engagement key to realising value and supporting development
Collaboratives rely on true commitment and partnership working, and the process of developing future plans – particularly when involving delegation to a lead provider – will test the strongest of relationships.
Trust among collaborative providers is critical. So too are relations with key system partners, particularly local authorities, at place and at the level of the ICB itself. These relationships need to be cultivated through focused outcome-driven work, starting with the mapping and analysis of all internal and external stakeholders and the development of action plans.
This concept is at the heart of the influence model developed by McKinsey's Emily Lawson and Colin Price.
The other key aspect of cultivating stakeholder relationships is to support effective decision-making. To make the best decisions, boards must engage with a wide range of partners and stakeholders and involve them in decision-making, and the same applies to provider collaborative boards. How can they design voice of relevant stakeholder into their decision-making structures in a way that is appropriate, proportionate and efficient?
Some of the common pitfalls we have seen are:
- Purpose and alignment: lack of alignment around purpose and aspirations – unable to answer the question ‘why are we doing this?’
- Culture: historical competition and/ or incompatible ways of working driven by different structures, culture, working practices, budgets and constraints
- Accountability: e.g. tensions between shared accountability and remaining single organisational responsibilities
- Complexity: unnecessary managerial complexity, e.g. organisations belonging to multiple provider collaboratives with no compelling reason
- Stakeholders: lack of support from key stakeholders.
So what can be learned by good practice?
Purpose and alignment
One of the common factors among more mature provider collaboratives is well-developed system relations. This is often either because of historic collaboration – formal or informal – a genuine concerted investment of effort, or a bit of both. Where these relationships have been cultivated, the following activities have usually been undertaken.
- succinctly defining their purpose, ensuring it is aligned with the system
- building strategies, objectives and work programmes, mindful of the four key aims
- linking the relevant system specific aims and objectives set in the integrated care strategy and joint five-year forward plans
- ensuring system input from broader partners, and other collaboratives, in the development of their guiding objects
- engaging with collaboratives beyond their system to share learning.
Collaboration and consensus
Successful provider collaboratives have also spent time and used a number of models to cultivate relationships, build consensus and lay the groundwork for genuine collaboration, not just cooperation. These models include:
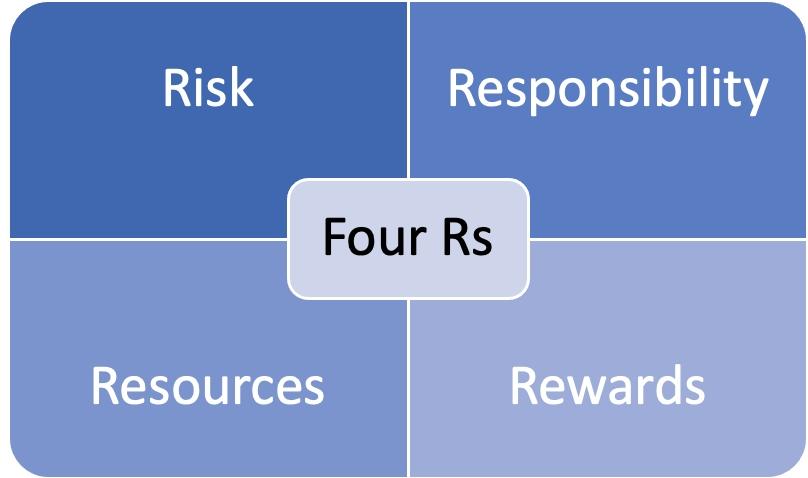
Arthur Himmelman and Aubrey Mendelow's collaboration continuum and the Four Shared Rs of Collaboration, to:
- illuminate organisational and individual perceptions on the maturity of the collaboration
- clarify ambition with regard to the depth of collaboration
- tease out what may be the missing ingredients to close the gap between current reality and future aspiration.
Connectivity and trust
The more developed and mature provider collaboratives have focused on their connectivity to the system and building trust. They have looked at how and where they need to link in, build collaborative relations, develop influence and trust and establish information flows.
They’ve done this through:
- formal governance
- direct links with the ICB
- informal links (e.g. for chair/vice-chair of collaborative)
- membership of other ICB committees and groups.
Influence
These provider collaboratives see communications and engagement as key to contributing to their influence in the system at both place, with the other provider collaboratives, the ICB and other critical partners. They see this influence as important social capital
Strategic stakeholder analysis and engagement
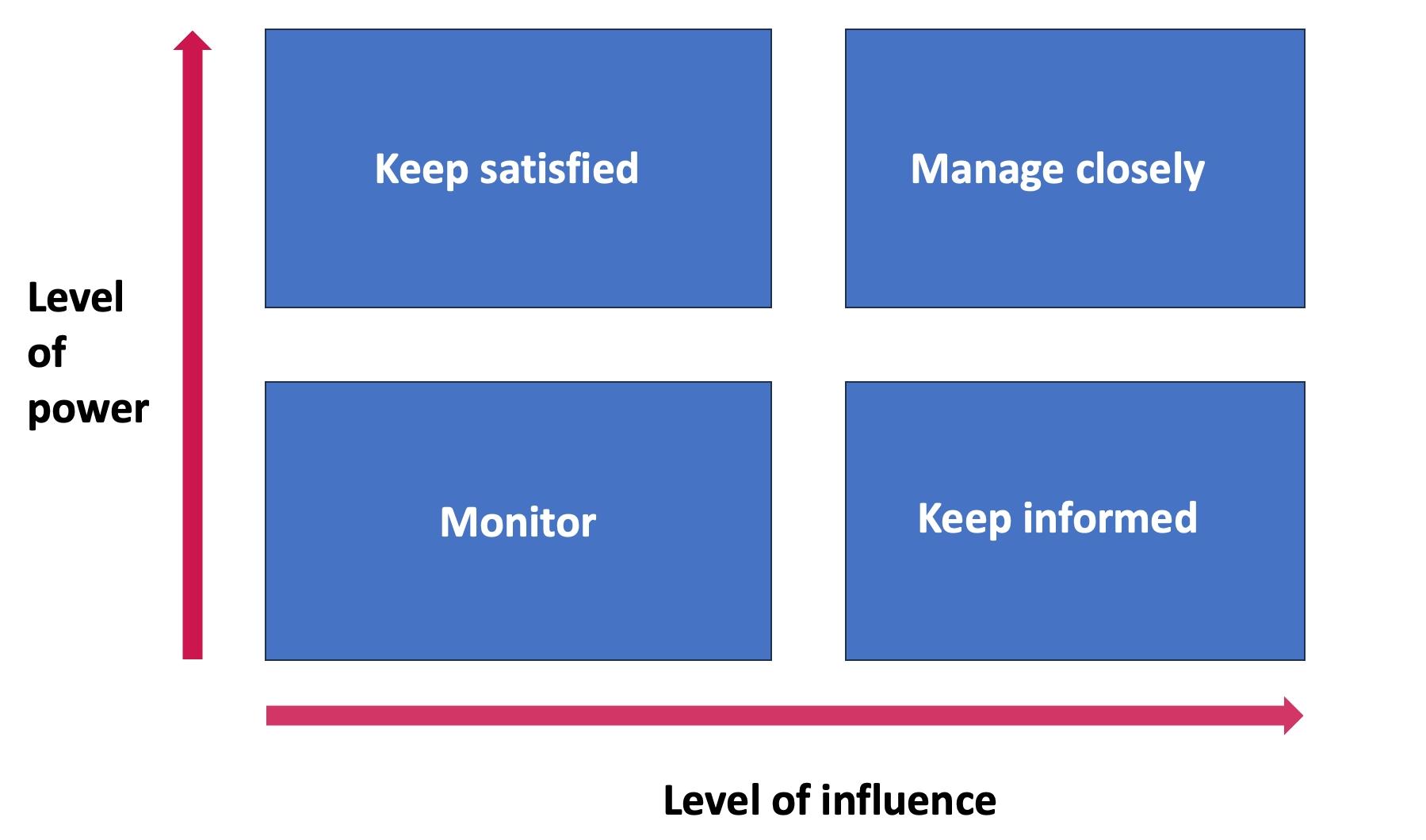
They have properly invested in stakeholder management, taking the time to properly map and analyse their key stakeholders – internal and external, strategic and operational –developing management and messaging plans for each and using this analysis and maintaining oversight of the key relationships.

Reflective practice
Some questions we think all collaborative leadership should reflect on are:
Internal
- How do we want the provider collaborative and its work to be perceived by our member organisations? How are we managing this perception?
- What are the key messages to our provider collaborative membership? What do they need to know about who we are, what we do, and how we represent them?
- How can we support the voice of our members in the ICB, ICP and across our places?
- What opportunities are we going to provide for our members to feed into the work we do? How are we going to capture their input and ensure it is fed into the system?
External
- How do we want our work to be perceived by the rest of the system (ICB, ICP, places)?
- Who are the key individuals and groups we need to reach?
- How can we build our visibility, influence and relationships in these areas and with these key stakeholders?
- What are our key messages to the rest of the system about our work and our role?
Recipe for success
There is a recipe for success for provider collaborative stakeholder engagement, which involves addressing the following:
- Maintain system and citizen focus
- Work on a clear vision and measurable outcomes for the local population
- Reach consensus on aims, scope and remit of collaborative
- ‘Try by doing’, and use informal arrangements where possible
- Focus on development of the partnerships and relationships required
- Sustain engagement efforts
- Adopt an incremental approach to development of governance arrangements.
GGI provides tools and frameworks to help manage relationships with system stakeholders. We also offer 360° reviews, which help identify issues and opportunities for strengthening relationships.
Our engagement consultants support the co-development of strong compelling narratives for individual organisations and systems. For service transformation, we offer ‘design thinking’ workshops, during which we rapidly iterate through new service models, co-designed with local people, health and care workforce, and provider partners.
For more information and examples of our work, please contact Daniel Taylor.
